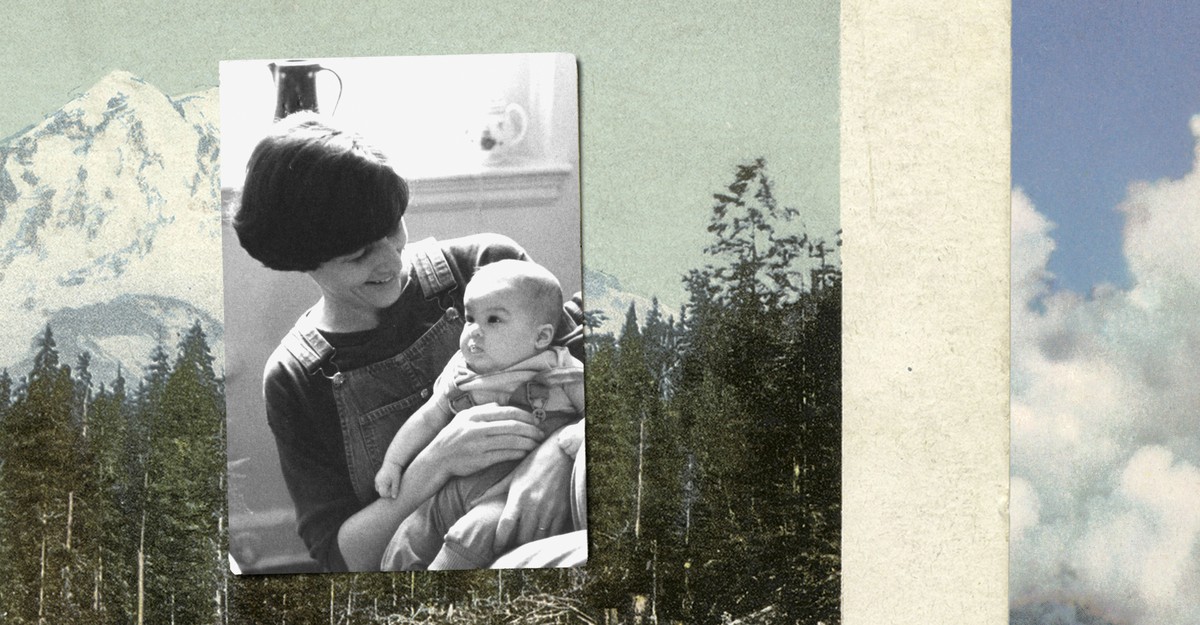
My mom could always leap into the coldest water. Every summer when we visited my grandma in upstate New York, my mom dove straight into the freezing lake, even when the temperature outdoors hit the 50s. The dogs, who usually trailed her everywhere, would whine in protest before paddling after her, and the iciness left her breathless when she surfaced. “Just jump, Lil,” she’d yell to me, laughing, before swimming off to vanish into the distance.
But I never could. I didn’t think much about that difference between us, until I flew north to be with her on the day she’d chosen to die.
When my mom found out in May last year that she had pancreatic cancer, the surgeon and the oncologist explained to our family that cutting out her tumor might extend her prognosis by about a year; chemotherapy could tack on another six months. A few days later, my mom asked if we could spend time together in Seattle over the summer, if we could get lemonade at the coffee shop while I was there, if I wanted to play Scrabble before I left. “Yeah, of course,” I said. “But—” She interrupted me: “I’m not getting surgery.”
After a decade of Parkinson’s disease, my mom already experienced frequent periods of uncontrolled writhing and many hours spent nearly paralyzed in bed. That illness wounded her the way losing vision might pain a photographer: Throughout her life, she had reveled in physicality, working as a park caretaker, ship builder, and costume designer. Now, plagued by a neurological disorder that would only worsen, she didn’t want to also endure postoperative wounds, vomiting from chemo, and the gloved hands of strangers hefting her onto a bedpan after surgery. Nor did she want to wait for the pain cancer could inflict. Instead, my mom said, she planned to request a prescription under Washington’s Death With Dignity Act, which allows doctors, physician assistants, and nurse practitioners to provide lethal drugs for self-administration to competent adult residents with six months or less to live.
As a doctor myself, I’ve confronted plenty of death, yet I still found myself at a loss over how to react to my mom’s choice. I know that the American tropes of illness—“battling to the end,” “hoping for a miracle,” being “a fighter”—often do harm. In clinical training, none of us wanted to unleash the fury of modern medicine upon a 98-year-old with cancer who’d just lost his pulse, but we all inflicted some version of it: ramming his purpled breastbone against his stilled heart, sending electricity jagging through his chest, and breaching his throat, blood vessels, and penis with tubes, only to watch him die days later. I didn’t want that for my mom; I had no desire for her to cling futilely to life.
And yet, even though it shamed me, I couldn’t deny feeling unnerved by my mom’s choice. I understood why she’d made it, but I still ruminated over alternate scenarios in which she gave chemo a shot or tried out home hospice. Though her certainty was comforting, I was also devastated about losing her, and uneasy about how soon after a new diagnosis she might die.
My mom had made her end-of-life wishes known by the time I was in fifth grade. Our rental home still held the owners’ books, among them Final Exit, a 1991 guide for dying people to end their lives. The author dispensed step-by-step advice on how to carry out your own death, at a time when nothing like the Death With Dignity Act existed in any state. When I found the book, my mom snatched it away. But months later, after her best friend died of brain cancer, she asked if I remembered it.
“If I ever get really sick, Lil,” she said, “I don’t plan to suffer for a long time just to die in the end anyhow. I would take my life before it gets to that point, like in that book. Just so you know.”
After her Parkinson’s diagnosis, my mom moved across the country to Washington, mostly to be near my sister, but also because in 2008, it became only the second state to approve lethal prescriptions for the terminally ill. Since then, despite much contention, the District of Columbia and eight more states have followed—including California, where I live and practice medicine. No dying patient of mine had ever requested the drugs, so I didn’t think much about the laws. Then my mom got cancer, and suddenly, the controversies ceased to be abstract.
Proponents of aid-in-dying laws tend to say that helping very sick patients die when they want to is compassionate and justified, because people of sound mind should be free to decide when their illnesses have become unbearable. Access to lethal medications (which many recipients never end up using) lets them concentrate on their remaining life. I sympathize: I’ve seen patients who, despite palliative care, suffered irremediable existential or physical pain that they could escape only with sedating doses of narcotics.
But I grasped the other side of the argument as well: that self-determination has limits. Aid-in-dying opponents have said that doctors who hasten death violate the Hippocratic Oath. Although I disagree with these moral objections, I do share some of the antagonists’ policy concerns. Many worry that state laws will expand to encompass children and the mentally ill, as they do in countries such as Belgium and the Netherlands. They argue that a nation that still devalues disabled people needs to invest in care, rather than permit death and open up the risk of coercion. So far, Americans who have used these laws have been overwhelmingly white and college-educated. But I could imagine patients of mine requesting death for suffering that’s been amplified by their poverty or uninsurance.
These policies are so polarizing that people can’t even agree on language. Detractors refer to “assisted suicide,” or even murder, while supporters prefer medical “aid-in-dying,” which I’ll use, because it’s less charged. But I don’t much like either term, and neither did my mom. She was already dying, so she didn’t think of her death as suicide. Nor would she accept a passive term such as aid-in-dying, when she was the one taking action. Lacking any suitable word, she settled on a phrase that felt stark but honest. “When I kill myself,” she’d say. When she killed herself, we should give her spice rack to a friend. When she killed herself, we shouldn’t hold a funeral, because that would be depressing. Her tone was always matter-of-fact. My stomach always somersaulted.
That summer, I read constantly about aid-in-dying—accounts of its use in Switzerland, essays in American medical journals, articles written by people who’d lost a loved one that way. I was the exception in our family. My mom was concerned with bigger issues, like whether the ice-cream shop would restock the lemon flavor before she died. My sister thought I was overintellectualizing things—and she was right. Sometimes we do the only thing we know how to, to keep from falling apart.
So I kept looking for the solace of stories that felt as complicated as my own thoughts. They were remarkably rare. To me, loving my mom meant acknowledging my own hesitation yet still respecting her measure of the unendurable. Juggling these emotions felt nuanced, but most of what I read didn’t. So many narratives cast aid-in-dying as either an abomination or the epitome of virtue, in which a dying person could be rewarded for courageous serenity with a perfect death.
Another daughter whose mother pursued aid-in-dying spoke in a TED Talk of the “design challenge” to “rebrand” death as “honest, noble, and brave.” But however tantalizing the prospect, the promise that we can scrub death of ugliness felt dangerously dishonest. Death can be wrenching and awful no matter where and how it happens: on a ventilator in an intensive-care unit, on morphine in hospice, or with a lethal prescription at home, surrounded by family. Being able to control death doesn’t mean we can perfect it.
The myth of the “good death”—graceful and unsullied, beatific even—has infiltrated the human subconscious since at least the 15th century, when the Ars Moriendi, Christian treatises on the art of dying, proliferated in Europe. A translation of one version counsels the sick on how to die “gladly.” The moral in these texts bludgeons you: How you die is a referendum on how you lived, with only a picturesque exit guaranteeing repose for the soul.
The notion has seeped through generations. “I hope if I’m ever in that situation, I’d have the bravery to do that,” one friend said about my mom’s choice. “It’s good she’ll die with her dignity intact,” said another. My mom’s physicians, kind and smart people, seemed so eager to validate her decision that the aid-in-dying criteria distilled to a checklist rather than unfurling into conversation. Even the name of the law my mom intended to use, Death With Dignity, implies that planned death succeeds where other ways of dying don’t. More than half a millennium after the Ars Moriendi, we still seem to believe that you can fail at death itself.
One doctor told us of a landscape architect who drank the fatal cocktail while exulting in her garden in full bloom. It sounded perfect—except that in all my years as a doctor, I’ve never seen a perfect death. Every time, there’s some flaw: physical discomfort, conversations left unfinished, terror, family conflict, a loved one who didn’t get there in time. Still, my sister and I tried to stage-manage a beautiful death. We booked a cabin in Olympic National Park for my mom’s exit. We would bake her famous olive bread and cook bouillabaisse. We’d wheel her to the beach, then to the towering cedar forest, then massage her feet with almond oil while we talked in front of a woodstove. The fireside conversation would be our parting exchange of gifts, full of meaning, remembrance, and closure.
As our family waited for that day to come, we kept thinking we should be tearing through a bucket list. Instead, we did what we always had—cooked, played games, read. We just did it with an ever-present sense of countdown, in an apartment where nearly everything would outlive my mom: the succulent on the windowsill, the lasagna in the freezer she made us promise to eat when she was gone.
My mom did have the lemon ice cream again, but our family never made it to the cabin in the forest. A month before the planned trip—10 weeks after my mom’s diagnosis—the pharmacy compounded the drugs: a mixture of morphine and three others. The bottle was amber, filled with dissolvable powder and labeled with the words No Refills. (“Now that would be a dark Saturday Night Live skit,” my mom told me.) The next morning, a Thursday, she called, dizzy and miserable. She wanted to die ahead of schedule, on Saturday. I got on a plane.
My mom, my sister’s family, and I spent Friday grilling chicken and drinking good wine. After my older niece painted my mom’s nails lavender with polka dots, the kids and my brother-in-law said their goodbyes and left. The next morning, my sister and I laid out the backyard like a set: a couch swathed in blankets. Tables with plants and photos and huge candlesticks. A stereo to play the music of our childhood and her motherhood.
But our revised choreography couldn’t erase how horrible my mom felt that morning, dispirited by her disease and deeply exhausted. We had to cajole her not to die in bed. Eventually, she came outside, where we drank peppermint tea and talked about nothing memorable. When the moment came to gulp the bottle’s contents, mixed into lemonade, she didn’t hesitate.
“You would make the same choice if you were me, right?” she said, setting down the empty bottle. I knew she wasn’t second-guessing. She was ending her time as our mother not out of lack of devotion, but because all other options felt untenable, and she needed confirmation that we knew this.
“Yes,” my sister said, “I would.”
“Me too,” I said—but in truth, I didn’t know. Maybe I would have dwindled over months of chemo as I learned to reshape my life in the face of imminent death. Maybe I would have died in hospice, surrendering myself to the fog and mercy of morphine. Maybe I would have stowed the drugs in a cupboard, cradling them occasionally and then, unable to reconcile the simplicity and complexity of that ending, replacing them. Each of these paths would have demanded its own form of courage—just not my mom’s type.
“I’ll just go to sleep now, right?” she asked.
“Yeah, Mom, you’ll just go to sleep,” I said. “I love you.”
My sister and I kissed her forehead, her cheeks, her collarbone. We avoided the poisonous sheen on her lips, where our tears had wet the residue of white powder.
The aspens rustled, confetti of silver. My mom didn’t cry, and the slightest trace of a smile alighted on her face.
“Bye,” she said. “You’ve been awesome.”
And then she dove off the dock. Her lips blued, and when she tried to speak more, the words never surfaced.
It took her five and a half hours to disappear completely, while my sister and I tamped down growing worries that the drugs hadn’t worked. My mom felt no pain—she couldn’t have, after all that morphine—but her passing wasn’t a fairy tale. Her suffering wasn’t embossed in meaning; she didn’t tile over her bitterness with saintly forbearance. My mom died on the day she was ready and by the means she chose. All of that matters, immensely so. She also died precipitously, far from the forest she’d dreamed of, while my sister and I were left with little closure and a prolonged, confusing death.
Usually, I write when I’m most upset, but my mom’s death catapulted me into a frightening depth of wordlessness. Weeks passed before I realized that my problem was not that I couldn’t find words at all. It was that I couldn’t tell the tale I felt I was supposed to. In that myth, death has a metric of success, and that metric is beauty. The trouble is that you can’t grieve over a version of events that never happened. You can only grieve over the story you lived, with all of its ambiguities.
My mom’s death was beautiful. It was also terrible, and fraught. That is to say, it was human.




