An experimental cancer drug could make thinking easier for individuals with Rett syndrome, a rare disorder linked to autism, according to new research from the University of California San Diego.
The discovery that could lead to therapies for patients with other neurological conditions.
The findings, published in Stem Cell Reports, highlight the role of microglia — a type of white blood cell found in the central nervous system — in the formation of the human brain.
Pinar Mesci, Ph.D., the study’s lead researcher, said: “very little information has existed on [the role of microglia] in early stages of neural development.”
This is because access to foetal tissue is limited, Mesci added.
In a bid to better understand their function, Mesci instead used brain organoids — “mini brains,” essentially, that mimic the developing brain of an embryo — grown from skin-derived stem cells of consenting patients.
Such organoids were created from individuals with Rett syndrome — a disorder primarily found in females that features loss of speech, purposeful use of hands, mobility and muscle tone, among other symptoms — as well as from neurotypical individuals.
Mesci then added healthy microglia to the Rett syndrome brain organoids and found that the functioning of synapses — where neurons connect and communicate — was “rescued.”
This occurred due to the restoration of phagocytosis, a process by which microglia — sometimes referred to as the “janitors” of the central nervous system — ingest and destroy foreign substances like bacteria and dead cells, keeping the brain and spinal cord tidy.
The process also involves “pruning” of synapses, which optimizes brain function.
Researchers also found that the synapses of typical neurons experienced impaired functioning when Rett syndrome microglia were introduced, further confirming the role of the immune cell in brain function and development.
UC San Diego School of Medicine professo,r Alysson Muotri, Ph.D., is the study’s senior author and director of the university’s Sanford Stem Cell Institute’s Integrated Space Stem Cell Orbital Research Center.
The researcher said: “If the brain’s ‘janitors’ are not working, problems start to arise.”
Faulty microglia make cognition even harder for Rett syndrome patients, who already contend with fewer and impaired synapses and dysfunctional astrocytes due to a loss of function in the MECP2 gene, implicated in other types of neurodevelopmental conditions as well.
Microglia with loss of MECP2 function “are not as good at pruning synapses and shaping the neural network — they don’t do a good job,” Muotri said.
The team then tested a battery of existing drugs on the microglia, to see if any might restore phagocytosis.
They found one: ADH-503, also known as GB1275 — an experimental oral pancreatic cancer medication that also reduces the number of immune-supressing cells that enter a tumour.
Other studies on Rett syndrome have highlighted potential therapeutic targets.
But none so far have identified a potential treatment involving human microglial cells.
By the time Rett syndrome patients are diagnosed, it’s too late to repair and not currently possible to replace faulty neurons, the primary issue in the disease.
Mesci said: “But by focusing on other cell types — and potentially finding drugs that improve how they work — we might improve the environment for those neurons and ease functioning for patients.
“That’s what I’m excited about.”
Jonathan Kipnis, Ph.D., is professor of pathology, immunology, neurology, neuroscience and neurosurgery at Washington University School of Medicine in St. Louis and director of its Brain Immunology and Glia Center.
He said: “I hope this work will ‘move the needle’ and bring the Rett community back to neuroimmunology.
“Understanding neuro-immune interactions in this complex disease may not only provide new insights into the disease biology, but also develop novel approaches to attenuate its progression.”
The research represents the first successful integration of human microglia into Rett syndrome brain tissues in vitro — a model that may prove superior to mouse models.
The researchers hope the study “opens doors for therapies,” not only for those with Rett syndrome, but for those with other neurodevelopmental and neurodegenerative disorders in which microglia play a role.
“That’s my wish,” Mesci said, “that we can improve quality of life.”
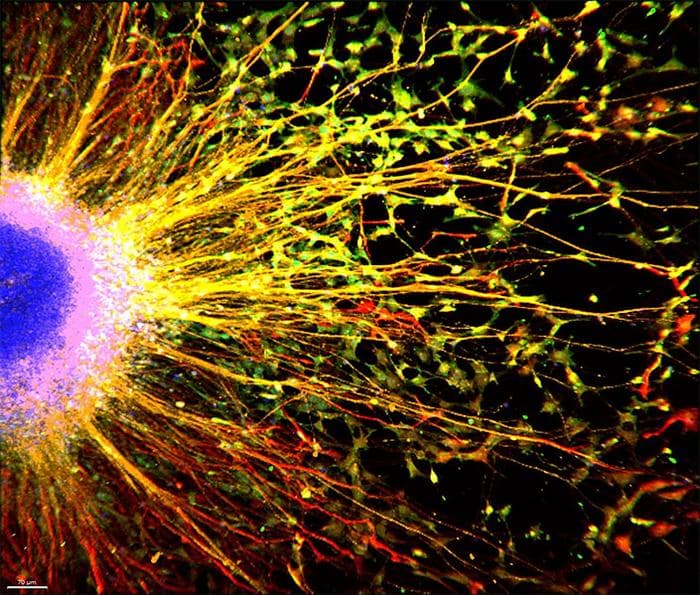
Muotri Lab/ UC San Diego Health Sciences



